After proving their worth in the aftermath of Hurricane María, thanks to philanthropic support, health centers are now being considered in the government’s disaster recovery plan for funding.
By Mc Nelly Torres | Centro de Periodismo Investigativo
Three days after Hurricane María, Isolina Miranda stared in disbelief at what was left of the two-story building where a community health center once stood in the heart of San Lorenzo, a town of 37,000 people in the eastern central region of the island.
Miranda is the executive director of COSSMA Inc., one of 20 community health centers in Puerto Rico.
María made landfall on Sept. 20, 2017. The hurricane’s powerful winds ripped off the health center’s sheet-metal roof and the rain damaged everything inside — medications, furniture, computers, medical equipment and a newly renovated obstetrics area.
When she arrived at the now-ruined center, she found patients and staff anxiously waiting. The patients worried about the clinic’s ability to provide medical services after the building was gutted; the staff were concerned about losing their jobs.
“People were crying,” Miranda said as she herself tried to control her emotions, but her eyes got watery nonetheless. “I told them not to worry… ‘Let’s see what we can do with what we have.’”
Miranda had seen the damage the hurricane had left behind on her drive to the clinic and suspected the need for health care services would be essential in the aftermath. She instructed the staff to set up a tent on the sidewalk and start documenting patients’ names and the medications needed as they arranged transportation for patients to other COSSMA clinics with still-viable pharmacies in nearby towns.
Health centers like COSSMA provide primary health care for impoverished populations in the island. But during the first days and weeks after María, these centers became the first responders for everyone who needed medical assistance and medications in their communities. The response by most of these health centers helped at a time in which a public health crisis unfolded and many hospitals were closed after the storm while federal and state government agencies — tasked to step in after a natural disaster — were not present to help bear the load, according to interviews with several people.
“We couldn’t communicate with anybody,” Miranda said describing the first few days after the storm. “We took our medical services to the communities.”
In many cases, health care providers such as COSSMA worked in tents set up outside the health center because the buildings were partly damaged or not safe, while others like Centros de Servicios Primarios de Salud de Patillas used their mobile units to visit patients at home, including some who lived in remote areas. The Corporación de Salud Asegurada Por Nuestra Organización Solidaria (SANOS) visited emergency shelters and elderly-care facilities in Caguas to provide primary care and medications for patients with chronic diseases, such as diabetes, hypertension, asthma and heart disease. The one in Patillas stayed open to the public even as the storm entered the island a few miles away.
These centers were also among the first to receive patients with conditions closely associated with catastrophic public health events such as acute infections, conjunctivitis, scabies, asthma, dermatitis and contagious diseases including influenza, dengue, leptospirosis and Zika.
“We were alone in the world,” said César Montijo, chief executive officer of SANOS, a health center in Caguas, when describing how his clinic stepped in to provide medical services and even food to communities in need 72 hours after the hurricane hit.
The health center’s unrelenting efforts at the time of the hurricane, showed that they are an effective part of the island’s emergency response strategy. Last year, the Health Resources and Services Administration (HRSA), the federal agency that provides funding for health centers, awarded $12.8 million to support preparedness, especially in remote areas. Direct Relief, a California-based organization that supports the immediate needs of victims of natural disasters, contributed funds to install solar panels in 37 clinics, and supplied pre-packaged modules with emergency medical supplies in advance of the 2019 hurricane season to 12 health centers. Other preparedness efforts have included: adding higher-capacity generators, installing fuel tanks large enough to store diesel for 21 days or more, building water storing systems and wells.
“We couldn’t communicate with anybody,” Miranda said describing the first few days after the storm. “We took our medical services to the communities.”
Last year, the government of Puerto Rico asked the U.S. Congress to approve $250 million in funds that would prepare community health centers’ response after a disaster and over a long term by supporting elements such as all-terrain vehicles and mobile care clinics that would be ready to respond in places with sustained damages and isolated areas after a disaster.
This was part of the government’s economic and disaster recovery plan. CPI asked the Department of Health of Puerto Rico to provide details on whether the funds were approved and a list of centers involved in these efforts and any emergency preparedness plan that includes health centers. But DOH forwarded the request to the Central Recovery and Reconstruction Office of Puerto Rico (COR3), and that office didn’t provide the information after repeated requests.
Medication and health care access vital after a disaster
Access to medications and medical services can quickly become a matter of life or death after a natural disaster, and this became apparent after the massive storm disrupted infrastructure — electricity, transportation, and communications — causing delays in access to health care, food, and water.
In Puerto Rico after María, those delays contributed to approximately 3,000 “excess deaths” between Sept. 20, 2017, and Dec. 31, 2017, according to the latest estimate by Harvard University.
The survey concluded that some of the reasons for the increased number of deaths after the storm included the inability to access medications, absent physicians and disruption to medical services, the need for respiratory equipment requiring electricity and the inability to reach 911, especially in remote areas.
Montijo said health centers focus on primary care became important at the time and it allowed hospitals to concentrate on more serious cases.
“We are talking about having medications that needed refrigeration, or providing therapy to asthmatic patients because they didn’t have any power at home,” Montijo said. “Those basic things are important and could be life-saving measures too.”
Arturo García, a physician and medical director at the health center in Patillas, said the clinic had many patients seeking comfort the night of the storm.
“We had a lot of people who came here to receive their respiratory therapy because they didn’t have any electricity,” García said, noting that they had prepared for that because the town has a growing elderly population. “People died here in Patillas because they didn’t have any electricity.”

Fifteen days after the storm, the 20 health centers and their clinics around the island were not mentioned on the daily fact sheet about the emergency works produced by the Federal Emergency Management Agency (FEMA).
The daily memos documented recovery efforts taking place every day by state health agencies and the U.S. Department of Health and Human Services, listing the number of hospitals, Centers for Diagnostics and Treatment (CDT) and urgent care clinics, according to a review of over a thousand pages of FEMA memos obtained by the Center for Investigative Journalism (CPI in Spanish), the result of a lawsuit filed against the federal government to obtain documents.
The daily memos did not include specific details about the health centers immediate needs such as electricity, water, medication and manpower or any efforts underway to provide relief. As far as FEMA’s documented memos, the community health centers and their role in providing primary health care to vulnerable communities did not exist.
“The government had multiple priorities, and at some point, the government, the Department of Health and FEMA decided to concentrate efforts on the hospitals,” said Alicia Suárez, executive director of the Association of Primary Health of Puerto Rico (ASPPR), noting that there was confusion about the community health centers. ASPPR is a support organization for the health centers in Puerto Rico.
In an email response to CPI request for comment, FEMA said it “supported the priorities established by the government of Puerto Rico and the Department of Health to determine the assistance to be provided to health care providers.”
“The P.R. Department of Health did not assign a response role to the 330s (health centers) in the relief operation,” Juan A. Rosado Reynes, a FEMA spokesperson wrote. “Therefore, any assistance provided to survivors was coordinated under their own initiative.”
Weeks after the event ASPPR began to impart a simple message to the government and FEMA: primary health care facilities are also important, Suárez said.
Nobody could have predicted the magnitude of the storm nor the devastation it left behind, not even the health centers that prepared for the hurricane. The challenges extended to the people who work in them: 95 percent of the centers reported staff who lost their homes.
Four weeks after the storm, 89 percent of the health centers were providing limited hours of operations and services because of lack of staff, electricity, and equipment, which prevented them from providing services like laboratory services, x-rays and dental among other services, according to a November, 2017 report by the Milken Institute School of Public Health. Sixty-five percent of the health centers required building repairs.
One of the federal mandates required health centers to continue their mission, regardless of the damages caused by the storm, to provide medications and primary health care services, without any restrictions, to those who needed the services after a natural disaster, Suárez said.
Serving underserved communities
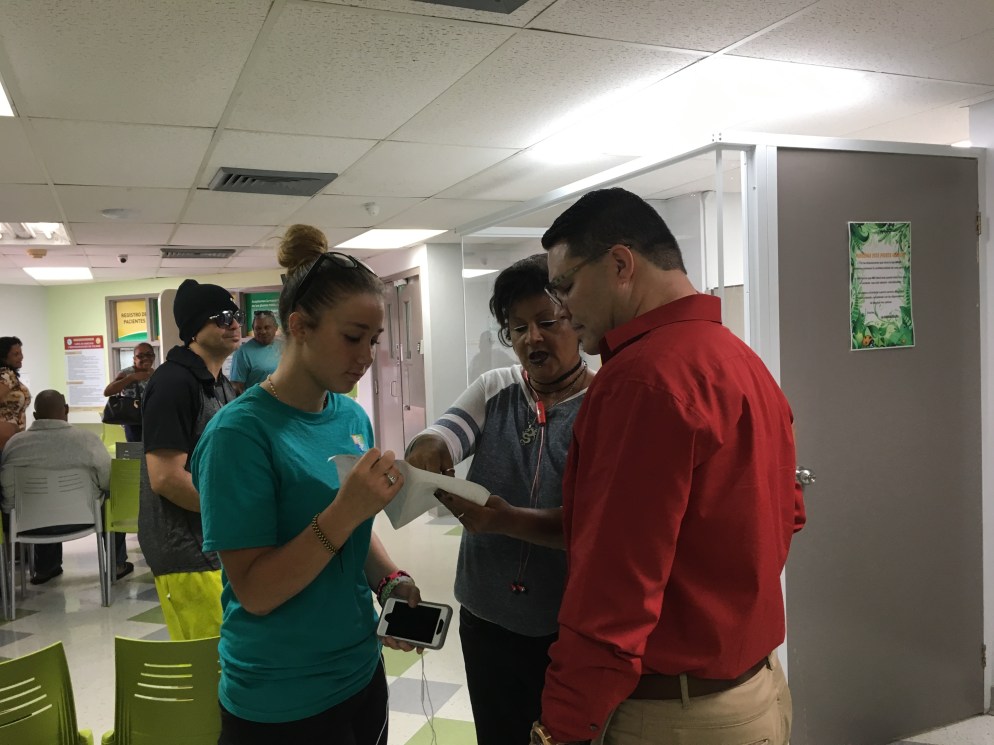
Salsa music blasted from the large speakers during a warm afternoon at the rural neighborhood of San Antonio in Caguas. SANOS’s mobile unit was parked in front of the neighborhood’s recreation center and it came packed that day with a family physician, a pediatrician and a nurse to receive patients all day. Patients, mostly elderly, waited inside the building where it was cooler, away from the sun.
SANOS provides primary health care services including pediatrics, vaccination, obstetrics, psychology, medication at a discount rate through a federal program and other services to about 7,000 patients annually.
“We respond to specific needs in the community,” Montijo said, noting that SANOS serves homeless, HIV and low-income patients whether they are part of the publicly-funded health program or not. “Every community has its own challenges and needs.”

The concept of community health centers emerged in the U.S. during the War on Poverty initiatives in the early 1960s, creating a model that targeted the roots of poverty by combining resources of local communities and federal funds to establish clinics in both rural and urban areas around America. Today, there are nearly 1,400 centers with more than 11,000 clinics in communities around the United States and its territories.
Known as 330s in Puerto Rico, because Section 330 of the Public Health Service Act is the federal statute that creates and authorizes the Health Center Program and its funding, these centers receive funds from the Health Resources and Services Administration (HRSA) program to provide primary care services in underserved areas. The health centers emerged in Puerto Rico in the 1980s.
In Puerto Rico, the 20 health centers have a total of 79 clinics, 10 mobile units and six programs in public schools in 59 municipalities, according to ASPPR. The health centers are all independent non-profit organizations, mostly federally-funded, owned by the communities they serve. A board of directors composed of its own patients governs each center and its clinics.
In 2017, the health centers provided comprehensive primary health care to more than 370,000 children and adults throughout the island. Most patients seeking their services receive Medicaid, but the centers’ clinics also provide care to people with private insurance, Medicare and people without insurance.
After the hurricane, three-quarters of the centers experienced a jump in the number of patients, according to a November, 2017 report by the Milken Institute School of Public Health.
“It became apparent there was a great need [for services] after the hurricane, especially from special populations,” said Rubén Rodríguez Bou, a family physician with SANOS who has been practicing medicine since 2004. “The lack of access to health care is a problem among the elderly population and this became prevalent after the storm.”
A week after the storm, Luis R. Rodríguez, a retired interior designer, walked to the San Lorenzo clinic and penciled his name on a notepad to get a ride to the COSSMA clinic in Las Piedras and get his diabetes medication. He had run out of medication after the hurricane and was lucky that his neighbor takes the same pills to control her type 2 diabetes. She shared some with him to tide him over.
“The bus was loaded with people,” he said.
Félix Ramírez, 65, who suffers from a heart condition, diabetes and needs oxygen to breathe, has been a long-time patient at COSSMA. When María hit, Ramírez was at Hospital Menonita in Caguas due to ongoing complications from a surgery he had in 2014. His wife Iris Vázquez, 58 and her 8-year-old grandson weathered the storm at a relative’s home in Caguas because they feared their wooden home in Barrio Hato wouldn’t be strong enough to survive the hurricane’s winds. It wasn’t.
Two days after the hurricane the hospital called Vázquez and told her that they were releasing her husband. Hospital staff had moved patients to the hallways as the hurricane destroyed the glass windows on several top floors and water rushed into the rooms.
Ramírez was on the sixth floor.
“Patients who were in delicate condition were sent home because the hospital was in no condition to keep them,” Vázquez said, adding that hospital staff was worried about bacteria infecting patients. “He has blood clots in his legs and emphysema, so patients like him were at risk.”
It didn’t take long for COSSMA’s medical team, including Ramírez’ own physician, nurse and a counselor, to show up at the house to check on his health. They also delivered medications on several occasions to her husband, but also insulin for her, Vázquez said during a phone interview.
Vásquez, who criticized the local and state governments’ slow response, said the clinics were lifesavers and they helped many even when they were operating from under an improvised small tent.
“The number of deaths would have been higher because many patients had chronic conditions and they needed medication,” she said about COSSMA’s work after the hurricane. “And my husband would have been on that list [of the dead] too.”
Today, the COSSMA clinic in San Lorenzo is operating from three rented portables across the street from where the old building used to stand. COSSMA also has clinics in Yabucoa, Humacao, Las Piedras, Aibonito and Cidra, serving a total of 30,000 patients with 300 employees.
“We see it every day when we visit patients at home,” said Yanira Rodríguez, a social worker for COSSMA. “It’s sad that after the hurricane we’ve seen that the needs have changed and even those who were taking care of an aging parent can’t do it anymore because of physical or emotional issues.”
Miranda rotates the staff between the clinics in San Lorenzo to Las Piedras and Humacao because they don’t have the space needed at the three portables to provide all the services the health center provided before the hurricane. Plans to start construction of a new clinic are underway.
Yanira Rodríguez, a social worker for COSSMA who is based in San Lorenzo, said mental health issues have been a growing concern as they’ve seen more patients who lost their homes and livelihoods suffering from stress-related conditions, anxiety, substance abuse and depression.
The most recent survey on the community health centers by the Henry J. Kaiser Family Foundation published in September 2018 validates Rodríguez experience. The health centers reported a “substantial uptick in patients suffering from depression and anxiety, including post-traumatic stress disorder (PTSD), and said their patients are more likely to experience suicidal thoughts and attempts than before the storm,” says the report.
Puerto Rico’s population is getting older and sicker suffering from chronic conditions — sometimes, with nobody to care for them — and there are also younger people with special needs. These vulnerable groups increasingly depend on public-funded programs at a time when deep divisions in the U.S. Congress and the Trump administration have delayed granting Gov. Ricardo Rosselló’s request for $600 million in emergency funds for the island’s food assistance program, which helps to feed 1.3 million families. Those funds are part of a package disaster bill approved this week that was signed by the president on June 6.
“We see it every day when we visit patients at home,” Rodríguez said. “It’s sad that after the hurricane we’ve seen that the needs have changed and even those who were taking care of an aging parent can’t do it anymore because of physical or emotional issues.”
Solidarity from U.S. health centers showed its face
As soon as the hurricane landed in Puerto Rico causing massive destruction, members of the National Association of Community Health Centers quickly organized to help health centers on the island. They partnered with the Hispanic Federation, Direct Relief and other community organizations to deliver help to health centers.
As communication gradually improved, reports from ASPPR began to arrive showing an urgent need for vaccines and drugs including antibiotics, eye drops, insulin, anti-inflammatory drugs, gastrointestinal drugs and respiratory therapy.
ASPPR set up a reporting system using WhatsApp to collect weekly data, sending updates on the health centers immediate needs to inform the Health Resources and Services Administration and other organizations ready to deploy help and support. The association used the same app to communicate with the health centers, but also visited many of the sites as conditions improved. ASPPR’s weekly reports helped other groups prioritize as well.
“If we couldn’t communicate, we would just drive to the location to evaluate the situation and that began the Monday after the storm,” said Darielys Cordero of ASPPR.
Each natural disaster brings its own unique challenges and lessons. Hurricane Katrina taught emergency workers that the response needs to be regional because people will always seek help at the local hospitals and health centers.
In Puerto Rico, people reacted in different ways depending on the individual situation, but health care providers at the health centers realized quickly that they needed to take health services to those who were unable to travel to the clinics. Some patients were too sick to travel, didn’t have transportation while others didn’t want to leave their damaged homes for fear to be robbed.
Feygele Jacobs, president and CEO of RCHN Community Health Foundation based in the Bronx, New York said private philanthropy was able to help with funding, medical equipment, manpower, medications and other necessities like toiletries.
“But what does it say when you are relying on private philanthropy [instead of the government]. Right?” Jacobs said.
Andrew MacCalla, emergency response director for Direct Relief, said the organization works closely with health centers in the U.S., including those in Puerto Rico. The organization landed seven days after the storm hauling $70 million worth of medications, half of which was donated to the health centers.
“We know that after disasters they (health centers) basically become first responders in their communities,” MacCalla said.
Challenges exposed in the community health centers
Regardless of the work, many health centers are struggling to recover from damages as they continue to provide primary health care to a growing poor and elderly populations. In 2016, 86 percent of the health centers patients on the island had below-poverty level income, compared to 70 percent of patients served by similar centers in the 50 states and D.C.
The hurricane might have exacerbated economic circumstances for many Puerto Ricans, including children and the elderly. According to a Washington Post-Kaiser Family Foundation survey of the island’s residents published in the fall of 2018, 29 percent of people surveyed earning $20,000 or more said they had lost income from a small business or missed days at work. Further, Puerto Rico presents the worst economic conditions for children in the U.S., including having the highest rate of children (56 percent) living below the poverty line and 84 percent living in high-poverty areas, according to the 2018 Kids Count Data Book released in 2018 by the Annie E. Casey Foundation.

Puerto Rico’s funding crisis and the island’s $70 billion debt have contributed to the decades-long migration of healthcare professionals. Hurricane María just made it worse.
At the island’s health centers, 90 percent of respondents said they had difficulties hiring physicians; 88 percent pharmacy staff; 67 percent substance abuse staff, and eight percent of the health centers indicated it was not possible to hire mental health and substance abuse staff at all, according to a survey of health centers published on April 2018 by the Milken Institute School of Public Health at George Washington University. More than half (57%) said it was difficult to retain staff, the survey shows.
Medicaid funding’s uncertain future
Puerto Rico’s healthcare system has been under financial stress for decades and Medicaid funding, which the island receives in the form of a block grant, was barely hanging by a thread before Hurricane María wrecked the island.
As part of the recovery efforts after the hurricane, the U.S. Senate approved $4.8 billion in Medicaid funds in early 2018, but this funding will run out in September of 2019.
This means that after September, the island would be facing a Medicaid funding shortfall and if Congress doesn’t act before, and that could leave 1.4 million people without health care, including most of the patients at the health centers.
Jacobs, who has collaborated with others to publish surveys about health centers in Puerto Rico, said the hurricane highlighted the health care funding disparities in Puerto Rico.
She noted that these centers are “doing extraordinary work, despite not having the ‘adequate’ funding.” She was in the island for the Three Kings Day holiday in 2018 visiting a health center in Loíza that was operating with a generator. “This bears some discussion because they are so at a disadvantage from the [U.S.] national point of view. They’ve been under-invested for decades.”
This article was produced as a project for the Dennis A. Hunt Fund for Health Journalism, a program of the USC Annenberg Center for Health Journalism.
This story was originally published on June 13, 2019 in English and Spanish by the Center for Investigative Journalism of Puerto Rico and its media partners.
















